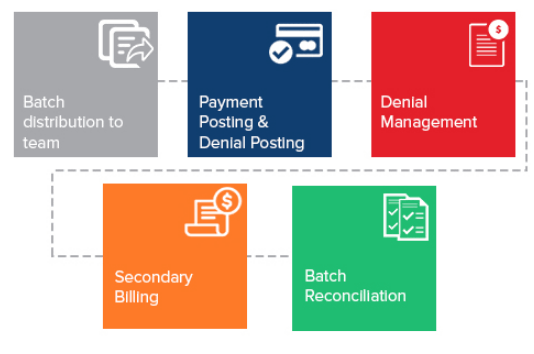
Payment Posting
A good payment processing team can provide critical insights into the overall effectiveness of your revenue cycle processes.
While many administrators look at coding and clinical documentation as the key anchors for effective medical billing and consider payment posting to be just the process of posting payments,
our remittance processing professionals not only process payments but provide you with trends and reasons for denials, prior-authorization, non-covered services, quality of your clinical documentation and coding processes, and effectiveness of your front-end patient collections.
We process the following types of remittance transactions with an exceptional degree of accuracy and timeliness:
Electronic Remittance Advisory (ERA) Posting. Electronic remittances typically contain a high volume of payment transactions. The processing of ERA batches involves loading the files into the revenue cycle system, processing exceptions from the batch runs by making due corrections using the functionality available on the revenue cycle system.
Manual Payment Posting. Payment information from scanned images of Explanation of Benefit (EOB) documents is captured and each line item is posted to the respective patient accounts. By developing practice and physician-specific business rules along with our team, we ensure accurate payments, adjustments, write-offs, and balance transfers.
Denial Posting. Our staff is conversant with ANSI denial codes as well as the remark codes used by different payers. We post denials into the customer’s practice management system and take actions such as billing the secondary payer, transferring the balance to the patient account, making adjustments/ write-offs as per defined policies, and routing the denied claims to appropriate work queues.
Posting Patient Payment. Patient payments should be accounted for in order to properly close the claim and avoid any inflated AR. We have extensive experience in processing payments received from patients via different channels like POS cash collections, checks, and credit cards (patient portals). Our payment processing professionals account for patient payments, make decisions on transferring any pending balances to secondary insurers, and resolve any credit balances submission, claim processing, charge capture, and enhance your overall revenue cycle efficiency!