A/R & Denial Management Services
Accounts Receivable Management
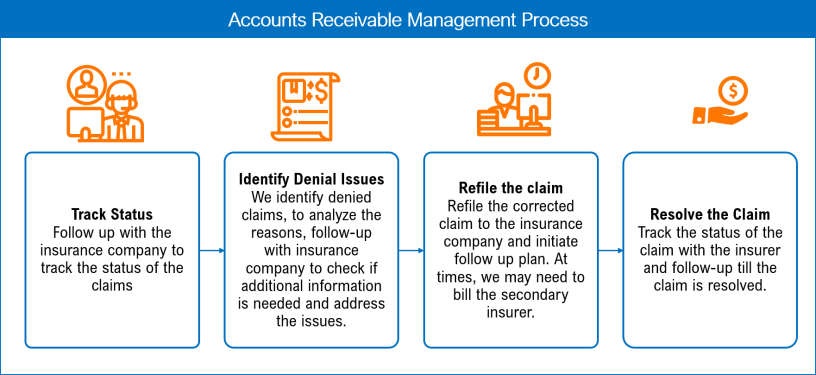
Issues with A/R will directly impact a provider’s margins, debt and organizational financial health. Therefore, A/R management is vital after claim submission and crucial for financial stability. It identifies the adjudication status of the submitted claim and helps in understanding the claim outcome. Early notification of a denial helps correct the claim at the initial stage and saves it from becoming ‘untimely’ for appeals or corrections. Our team will analyze your financials, identify errors and implement efficient processes to collect payments and clear backlogs of unresolved A/R within a quick turnaround time.
Our Accounts Receivable Management Services include:
~ Follow-up across all payers on outstanding A/R
~ Inherited A/R cleanup projects
~ Underpayment management
~ Denial management
~ Credit balance resolution
Denial Management
The average claim denial rate in the healthcare industry ranges from 5% to 10%. Most providers consider these denied claims as a drain on resources and negatively impact revenue. Many providers, however, do not realize just how significant that impact is. Data shows that 90% of denied claims are preventable and up to 65% of denied claims are never resubmitted, even though 63% of denied claims are recoverable. This is money left on the table. Our effective denial prevention strategy and dedicated denials team can help your organization increase payment recovery. This is done by identifying the root cause of denials, reworking the denials, writing appeals if necessary and resubmitting claims.
Our Denial Management Services include
~ Identifying and correcting root causes of denials
~ Contacting payers and patients to gather additional information
~ Preparing appeals, correcting claim information and resubmitting corrected claims