Revenue Cycle Management
Patient demographics
Patient demographic entry to ensure claims will be sent out and paid efficiently.
Provider Credentialing
Enroll providers with government and commercial payers and initiate and maintain accurate credentialing statuses and ensure timely and clean claim submissions.
Eligibility Verification
Meticulous eligibility and benefit verification to reduce claim denials due to incorrect billing and ensure better collection at first attempt.

Prior Authorization
Obtain quick and timely prior authorization before the care is rendered to ensure that authorization does not hamper patient care or physician billing.

Charge Entry & Claims Submission
Experienced billing staff that ensures clean charge entry with scrubbing of all claims for fewer denials and underpayments.
Payment Posting
Posts all payments, insurance or patient, and provides daily reconciliation
Account Receivables
Diligent submission tracking and follow up with the payers for quick payment processing and timely denial resolutions.
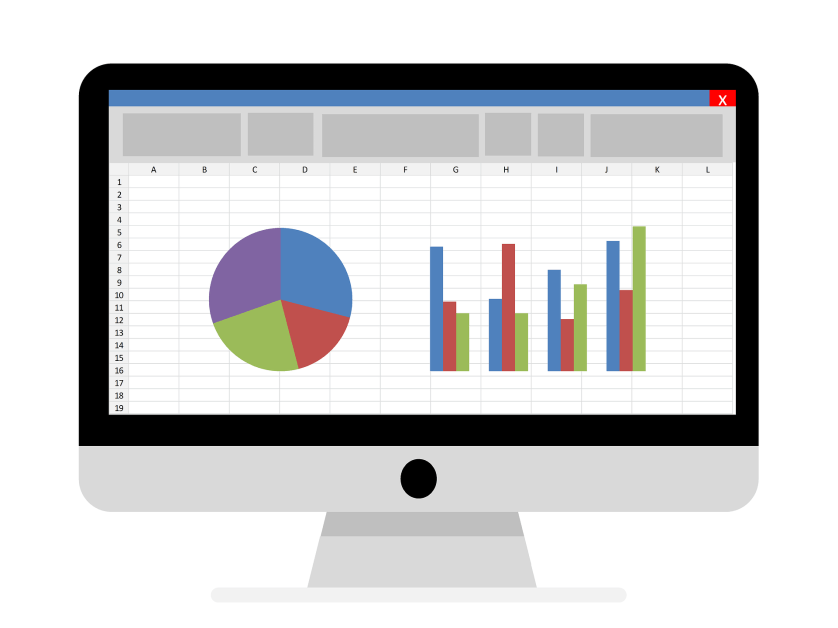
Reporting
Complete Reporting to provide clarity on claim status, payment projections, denials and adjustments.

